Chronic insomnia. Don’t sleep on it!
Insomnia symptoms, what are they really?
Do you struggle with your sleep night after night? Are your days difficult as a result of poor sleep? Does it take you forever to fall asleep? Do you wake up several times a night or very early in the morning and can’t get back to sleep? Do you have low energy and feel fatigue as you go about your daily activities? Is sleeping problematic for you?
Could it be acute or chronic insomnia symptoms?
Chronic insomnia presents as dissatisfaction with sleep quality and duration despite adequate opportunity and circumstances for sleep. It is a long-lasting condition and causes significant distress. Chronic insomnia is a 24-hour problem as it negatively impacts both night and day functioning.
Aside from sleep discontentment, people report one or more of the following nocturnal insomnia symptoms:
- Trouble falling asleep (initial insomnia or sleep onset insomnia) at bedtime. People can toss and turn for more than 30 minutes, past the usual time it takes to fall asleep. A few minutes to 30 minutes is considered normal.
- Trouble with staying asleep (Middle insomnia or sleep maintenance insomnia) at night, meaning waking up several times in the middle of the night or having trouble falling back to sleep after waking.
- Waking up too early in the morning (terminal or late insomnia or sleep offset insomnia) and being unable to go back to sleep.
Even if lack of sleep occurs as an insomnia symptom, insomnia is not a voluntary decision to cut back on sleep leading to sleep deprivation. Moreover, people who have insomnia are not short sleepers, since they don’t feel rested during the day, as natural short sleepers do.
A lot of us suffer from chronic insomnia, as it is the most common sleep disorder and affects us at any age (yes, children can suffer from insomnia). Women are twice as likely to suffer from it, and it is also more frequent in the older population. At least one person out of four (25%-30%) has insomnia symptoms once in a while, and as many as one person out of ten suffer from it chronically (10%-15%), regardless of age, children included!
Periods of acute insomnia are common as they are often a result of transitions during one’s life span. These short episodes of situational insomnia are considered normal, as both negative and positive events can explain them. Occasional nocturnal symptoms often occur when we are stressed out, under pressure, grieving, or coping with a change of routine triggered by life events, such as sickness, moving, use of drugs, planning an anniversary, pregnancy, menopause, etc. If this is your case, you should not worry too much as acute insomnia is not dangerous and it should not add to your current stress. Try not to overthink it and make “sleep on it!” your motto.
But if you are stuck in an insomnia pattern that lasts and is hard to break, don’t sleep on it, as there are things you can do about it. Maybe like a lot of people, you think that’s the way it is, but read on! Unlike what most people think, this is not inevitable. Solutions exist. No matter how old you are and no matter how long you’ve been suffering from insomnia, chronic symptoms can go away. For example, it’s not an expected sign of aging even if it is more common at this age (see “Sleep, a personal and lifelong natural need” and “Age-specific do’s and don’ts. Sleep on it!”). If you are 65 or older, there’s still a 70%-80% chance that insomnia can improve.
A crucial way to regain peaceful sleep is the will to change. Are you ready for a change or will you keep carrying this burden? The first thing to do is change your mind if you think, “It is what it is.” The second is to learn more about insomnia and sleep and what behaviours to adopt so you can break the vicious cycle you’re in. That’s what this website is here for, so you are off to a good start.
What to do or not do?
As a rule of thumb, overthinking and stressing about sleep is not a good thing to do, especially if you are prone to insomnia symptoms. It may sound contradictory since this website aims to raise awareness about the importance of sleep, sleep disorders and the health consequences of not having a good night’s sleep. However, there is a crucial difference between getting informed to take healthy decisions and worrying too much, being stressed or downright obsessed or frightened about a health matter. With insomnia especially, an anxious attitude is problematic as it contributes to a vicious cycle with insomnia creating more fear and anxiety of going to bed, doubts about one’s ability to sleep, an unhealthy sleep routine and behaviours that are not recommended for sleep hygiene, more sleeplessness, more sleep worries about not sleeping, and on and on.
Since chronic insomnia is strongly related to our sleep dissatisfaction and erroneous beliefs about it, the key to change lies within our self and how we think and act about sleep. Before acting on our vicious cycle inducing thoughts/behaviours or taking medication (prescribed, over-the-counter or self-medication such as cannabis or alcohol use), the cause of insomnia symptoms must be ascertained with a healthcare provider who is knowledgeable about sleep (physician, psychologist, pharmacist, lung and airway specialist, etc.) See next section for more on the causes and factors that trigger and perpetuate insomnia.
If your insomnia symptoms are occasional or linked to an emotionally loaded transitional period, to help ease this over time, remember to maintain a healthy sleep routine and hygiene to not fall into the vicious cycle of insomnia.
For example, stick to a regular sleep schedule (same bedtime and wake time) as much as possible so you don’t aggravate your daily symptoms, and do not overuse sleeping aids such as pills and alcohol to help you fall asleep, as they can reduce the recuperative function of your sleep (less slow-wave sleep) and create addiction. Bet on healthier choices and stress management: exercise during the day, take in as much sunlight or the equivalent as possible, eat well, talk about what’s on your mind and clear your head as much as possible before going to bed. Try to maintain a comforting sleep routine and maybe add relaxation techniques to it such as deep breathing prior to sleep. Talking about insomnia symptoms with your physician or psychologist may also help you cope with the underlying stressful situation and get situational help and short-term treatment.
However, if you experience symptoms several times a week and for as long as three months, your insomnia symptoms are considered chronic, and you should not hesitate to talk about it with your physician or psychologist as they are the ones who can help. Unfortunately, sleep disorders including insomnia are not yet well known by many healthcare practitioners. Most of them will rely on medication such as sleeping pills, in an attempt to help ease your sleep. However, for chronic insomnia, this is not the treatment of choice. That’s because it can only have a very short-term effect since we adapt to the effects of this type of medication, which necessitate higher dosages for example. Moreover, sleeping pills can even aggravate your condition since these medications can reduce slow-wave sleep, the type of sleep that helps us recuperate, and it may lead to addiction.
When in doubt, it is always good to count on a sleep clinic or a healthcare provider who is knowledgeable about sleep to get accurate information and diagnosis and the best therapeutic options.


To reach the right diagnosis, sleep experts will review your medical history and psychological well-being as well as sleep habits and sleep hygiene.
Sleep studies using polysomnography, PSG are often not necessary to diagnose insomnia but may be recommended to make sure it is not a consequence of any other sleep disorders, e.g. restless legs syndrome (RLS) or periodic limb movement disorder (PLMD) or sleep apnea.
A sleep diary is strongly suggested under professional supervision to target what needs to be addressed. Sleep professionals often use it as the first step to bring about changes in one’s sleep habits. It should be done for about a week or two to gather daily information about insomnia-triggering events, sleep hygiene together with sleep routine, estimated minutes to fall asleep, number of night awakenings and wanderings, and whether sleep is regular or not scheduled (bedtime and wake time).
The best treatment option these days, with a 70%-80% success rate within a few weeks, is cognitive-behavioural therapy for insomnia (CBTi). It has a much better rate of success and longer lasting effects compared to using sleeping pills. As mentioned, a willingness to change and get better is mission-critical to alleviate insomnia symptoms, making this psychotherapeutic option a natural fit. As with any big change in life, this one calls for dedication, as it may not be easy to change old unhealthy habits and ways of thinking. That’s why social support and guidelines are essentials. The help of a psychologist or psychiatrist is a must and the support of fellow insomniacs may also be helpful in some circumstances.
CBTi treatment focuses on psychological as well as behavioural factors that contribute to the vicious cycle that is chronic insomnia. It takes about two months, a small price to pay to sleep soundly when you think about it. The lasting success of this approach lies in its multidimensionality as well as the personal motivation to change. Here are some various aspects of insomnia taken into account during CBTi:
- Sleep awareness and education about sleep (see “What is sleep?” and the section on good sleep hygiene).
- A few psychotherapy sessions, individual and group, to address false beliefs and distorted, obsessive or anxious thoughts about sleep and insomnia.
- Daytime relaxation techniques to manage stress and increased brain activity (hyperarousal state) often seen prior going to bed. There are several methods, including meditation.
- Sleep restriction technique, which consists of limiting the time in bed not sleeping, tossing and turning. Ultimately, sleep restriction does not reduce sleep duration, it only decreases the time spent hoping to fall asleep. The new sleep schedule will be shorter, but sleep quality will increase.
- Specific stimulus control instructions:
- To create a positive association between bedtime and falling asleep quickly go to bed only when sleepy, not just tired but sleepy.
- Make it a habit after 15-20 minutes lying in bed not sleeping to get out of bed and do a non-stimulating or boring activity until you feel sleepy. Do mandalas, breathing exercises, etc. out of bed in a dimly lit room.
- Reserve the bed and bedroom for sleep and sexual activities only; no use of cell phones, tablets, television etc, no reading, and no problem-solving in your bedroom.
- Keep a strict regular sleep schedule, same bedtime and wake time each night. Be especially constant with wake time.
- Never look at the clock before your morning wake time or wake-up alarm.
- Never nap during the day, so you boost the sleep force called sleep drive, which is in part responsible for our need to fall asleep at night.
You can implement some of these recommendations on your own but remember that it has to be applied consistently and for a certain period of time to be successful and alleviate insomnia symptoms.
As most of us know, changing is not an easy thing to do, and most of us will need coaching to start and maintain lifestyle changes. You may understand very well the rationale for those CBTi recommendations, but you may need guidance to address problems, such as compliance, as they arise during treatment.
In other words, a web site or even an internet-based treatment may be the answer for some people, but those with more severe insomnia or motivation issues will most probably need direct guidance from a therapist trained in cognitive-behavioural therapy (CBT) to get rid of insomnia.
Also, if you suffer from mental health issues (depression, anxiety, etc) as well as insomnia, it is recommended to see them as distinct entities. Remember that it is not because depression/anxiety resolve that insomnia symptoms will go away. They are two separate but concomitant issues. They both require proper treatment at the same time or one after the other, as insomnia is a health issue in itself.
What are the causes of chronic insomnia?
We don’t fully understand insomnia, but it seems that before going to bed the brain is overactive, more active than it should be. This is a state called hyperarousal.
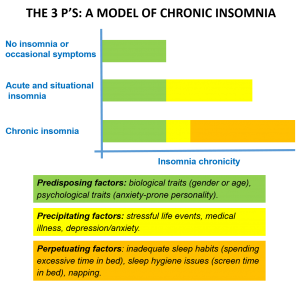
Keep in mind, however, that no matter what causes and triggers insomnia, symptoms are always related to the same individual factors. The latter have been divided into three categories called the 3 P’s model:
- Factors that put the person at risk – Predisposing factors
- Factors that are triggering the symptoms – Precipitating factors
- Factors that maintain the symptoms and contribute to the chronicity – Perpetuating factors.
We all have experienced one or more of these factors in our life. But it’s the accumulation of factors that becomes problematic and explains how acute and chronic insomnia sets in.
Predisposing factors are responsible for the occasional night of poor sleep whereas acute or situational insomnia symptoms are the addition of the predisposing and precipitating factors such as positively or negatively perceived stressful life events (e.g. pregnancy, separation, or death), which can trigger insomnia symptoms.
When insomnia persists over time, the 3 factors pile up. With time, the person will develop inadequate sleep beliefs, habits or hygiene that perpetuate the vicious cycle, and insomnia becomes chronic and will continue even with the removal or removal of the precipitating factor. Again this is why CBTi techniques are the way to go since they target those perpetuating factors.
The figure below represents the 3 P’s accumulation model explaining how insomnia symptoms set in:

What are the consequences of chronic insomnia?
Insomnia symptoms have significant immediate and long-term consequences affecting both our days and nights. Insomnia is responsible for exhausting night and day symptoms such as fatigue, lower energy, lack of concentration, mood swings, increased risk of work and car accidents, as well as a long-term negative impact on health caused by sleep loss.
The cumulative long-term effects of sleep deprivation and insomnia have been associated with a wide range of deleterious long-term health consequences including an increased risk of hypertension, obesity, depression, etc. (for more on the short- and long-term effects of sleep deprivation, see “Why sleep?”)
Insomnia is also a societal issue. The economic burden of insomnia is very high worldwide. Insomnia is taken seriously more and more by insurance companies. Many industries and several countries are now addressing it as a public health matter. In Quebec alone, a study published in 2009 estimated the total annual cost of insomnia at $6.6 billion, mostly attributed to insomnia-related work absences and reduced productivity. Society pays too. The economic burden of not treating insomnia is thought to be higher than the cost associated with providing effective treatment such as CBTi.
The general public and healthcare providers alike need to learn more about sleep, including sleep disorders such as insomnia, to make life better for everyone.